We don’t think so, but we’re convinced that much could be done to share cultural knowledge among health professionals who work with people from diabetes from culturally and linguistically diverse (CALD) backgrounds.
In an earlier blog, University of Melbourne Public Health postgraduate Sorayia Noorani wrote about the project she did as part of her professional placement with Fenton. Combining 16 in-depth interviews with health professionals and a desktop literature review, she investigated the influence of cultural factors on diabetes care and management. Secondary to this question was testing whether health professionals felt they would benefit from guidance on these cultural factors when working with people with diabetes from CALD backgrounds.
In this follow-up post, we reveal some project findings and recommendations while acknowledging the global struggle against diabetes marked by World Diabetes Day last weekend.
Qualitative research: interviewing time-poor health professionals in the field
In previous research we conducted on behalf of Diabetes Australia, our conversations with health professionals and people with diabetes suggested that culturally sensitive health professionals were better placed to help people from diverse backgrounds. In engaging Sorayia we hoped to test this premise for ourselves in an area of Victoria known for its community’s ethnic diversity and its diabetes prevalence: Brimbank.
We chose Brimbank because it has sizable Vietnamese and Arabic-speaking populations. Victoria’s Vietnamese communities are some of the largest and well-established, enjoying many attendant benefits such as networks of Vietnamese-speaking health professionals and community support groups. In contrast, Arabic communities represent a smaller but faster growing population with fewer options for Arabic-speaking health services.
This is central to the issue of trust between a patient and health professional: aside from using interpreters to overcome language barriers, a ‘mainstream’ GP who doesn’t speak Arabic must also navigate those cultural factors that could influence a patient’s ability to accept a diabetes diagnosis and their openness to advice about lifestyle and dietary change. For example, encouraging women from Arabic-speaking communities to exercise was reported as a particular challenge because cultural norms often dictate this as unacceptable female behaviour outside the home.
Contacting more than 60 clinics, we sought interviews with GPs and diabetes educators. Of the 16 interviewees, 11 were GPs and five were diabetes educators; four participants spoke Vietnamese and one spoke Arabic.
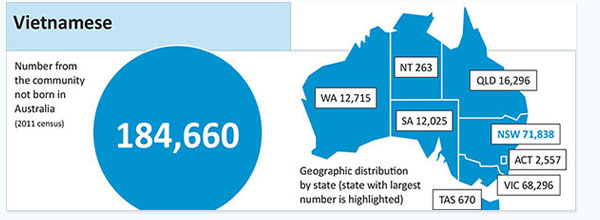
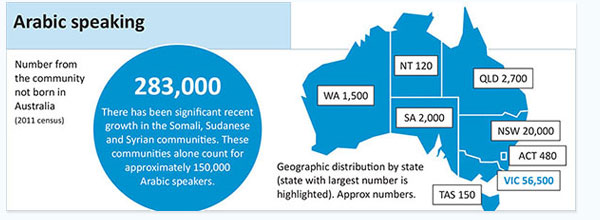
Charts profiling Vietnamese and Arabic language groups in Australia (Australian Bureau of Statistics, 2011 Census). Click images to view PDF versions with more detail.
Key findings
- 70 percent of participants said half of their patients with diabetes come from non-English speaking backgrounds.
- 55 percent agreed that they modified certain aspects of advice depending on a patient’s cultural background.
- 70 percent of participants said they vary the nutritional advice given to patients depending on their cultural background.
- 75 percent agreed that cultural factors have a significant impact on diabetes self-management, citing aspects like compliance with medication, embarrassment about having diabetes and accepting responsibility for self-management.
- More than half of participants that don’t speak Vietnamese or Arabic admitted to previously having consultations with patients where they felt having information about Vietnamese and certain Arabic-speaking cultures would have been useful.
- No participants knew of existing resources that provided cultural guidance information specific to diabetes care and management of patients from CALD backgrounds.
- 81 percent of participants said they would value or use resources with information about various cultures and how culture can impact diabetes care and management.
- A small number of participants had concerns that these resources could potentially encourage generalisations and cultural stereotypes.
Health professional quotes
“I adjust information depending on the cultural background of patient, particularly if I know or understand the patient's cultural background, I am able to link the chronic condition to their lifestyle and diet.”
“It makes a huge difference as most CALD patients are under the medical model where they are treated with medication and told to follow doctors orders. Not too many are familiar with the self-management model of health which is about taking control of your own health. Some cultures find this difficult to understand.”
“Yes, I think it would be really useful because a lot of diabetes educators and GPs have not had much experience with different cultural backgrounds. It is really important that they understand the culture not just assume people are going to do whatever Australia-born people do.”
Desktop review: the lack of diabetes-specific cultural guidance
Sorayia’s search and review of existing resources offering cultural guidance suggested that none of those currently available for health professionals carry information specific to diabetes management. A variety of translated resources are available for people from CALD backgrounds, but for health professionals, the review found only general information about cross-cultural practices to enhance cultural sensitivity and awareness within health care services – and many focus on the principles of being culturally sensitive without showing how to do it in practice.
Key findings
Below are the topics that participants felt would be the most important for providing cultural guidance.
- The way different cultures view diabetes.
- Eating habits, most common foods and diets of various cultures.
- Meal plans.
- Different approaches to encouraging physical activity.
- Issues around health literacy and understanding of health.
- Expectations from family and caring for children.
- Attitudes towards medication.
- Information about various cultural traditions and events such as Ramadan and other religious holidays that can impact diabetes management.
- Interviews with patients from different backgrounds exploring individual stories.
- Thoughts and feelings of the person with diabetes with a psychological care component.
- How to find an allied health service, particularly culturally diverse diabetes educators and dietitians.
Recommendations to increase cultural knowledge among health professionals
- Develop diabetes-specific cultural guidance resources
Resources should be developed in consultation with health professionals and community representatives, ensuring information is culturally sensitive and relevant while avoiding stereotypes. - Prioritise information related to food, lifestyle and physical activity, and cultural traditions, attitudes and expectations
Diabetes care and self-management, particularly type 2, is strongly associated with dietary and lifestyle changes. Providing information that enables GPs to give culturally appropriate advice on these aspects will be the most beneficial. - Keep materials up to date to include newly arrived CALD communities
Health professionals are least likely to have an understanding of recently migrated communities. Resources should be continually updated to include information on more recently arrived CALD communities. - Make materials adaptable for a range of health professionals
Diabetes care can involves a range of health and allied health professionals, from endocrinologists and GPs to podiatrists and nutritional professionals. Tailoring resources to these professions depending on the aspects of diabetes they address will ensure their relevance and value as practical tools.
By Alan Fitzpatrick and Sorayia Noorani